With the warm weather, comes an increase in sport activity. And with an increase in sport activity, we are seeing more sport related injuries in the clinic.
Concussions are unfortunately becoming more common; more than 23% of adolescents reported injuries 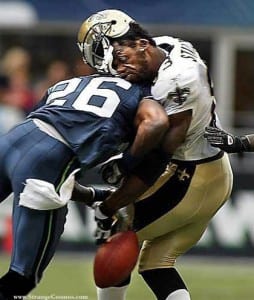 to their head in the previous year. With more youth playing sports, the rate of concussions has been increasing. Concussions can occur more often in young children as the head is proportionally larger to the rest of the body. In adults, the concussion rates tend to decrease, as the brain and head and more proportional in size.
to their head in the previous year. With more youth playing sports, the rate of concussions has been increasing. Concussions can occur more often in young children as the head is proportionally larger to the rest of the body. In adults, the concussion rates tend to decrease, as the brain and head and more proportional in size.
Concussions occur when there is a hit or blow to the head, causing injury to the blood vessels and nerves of the brain. The injury can be called brain trauma and can cause a wide range of symptoms. Concussions can be hard to spot. Sometimes you may see a bruise at the site of impact, but other times the signs and symptoms may not show up until a few days later. Even the symptoms may vary in length from a few seconds to a few days.
Here are a few signs to look for:
The severity of the concussion can vary; concussions are graded from 1 to 3: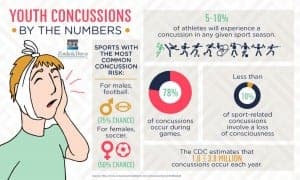
What should you do if you suspect a concussion?
Chiropractors help manage concussions regularly. As a primary care provider, chiropractors are often the first health practitioner to be seen by a patient after their injury.
Chiropractors use a specific assessment tool called the Sport Concussion Assessment Tool 2 (SCAT2) to evaluate, assess and manage concussions in athletes. This assessment tool is used to evaluate symptoms, physical signs, Glasgow Coma Scale, sideline assessment using Maddocks score, cognitive assessment, balance, and coordination.
Because a concussion is a brain injury caused by a direct blow to the head, neck or face, there’s a good chance that the blow has caused a misalignment of the cervical spine. This is similar to whiplash. A chiropractor can evaluate whether you demonstrate signs of neck injuries commonly associated with concussions, and provide you with relief of neck pain and cervicogenic headaches.
Additional guidelines your chiropractor will give you for concussion include no alcohol, aspirin, anti-inflammatory medications, and sleep agents should be taken. Use Tylenol for pain if necessary. Do not drive until you can return to the sport.
Shane, E.R., et al. Sports Chiropractic management of concussions using the Sports Concussion Assessment Tool 2 symptom scoring, serial examinations, and graded return to play protocol: a retrospective case series. Journal of Chiropractic Medicine 2013 (12): 252-9.